CHARACTERIZATION OF CYSTIC PANCREATIC LESIONS ON EUS, A SINGLE CENTRE EXPERIENCE
DOI:
https://doi.org/10.55519/JAMC-01-12832Keywords:
Pancreatic cystic lesions; EUS; EUS-FNAAbstract
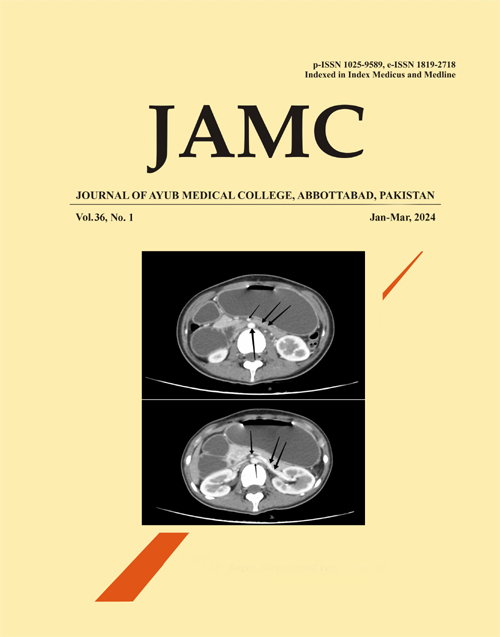
Background: Pancreatic cystic lesions are increasingly diagnosed these days due to better imaging techniques. It is important to detect the lesions and perform a detailed analysis as some of them are potentially malignant. Methods: From April 2023 to September 2023, all patients with recurrent and/ or persistent abdominal pain lasting for more than a week were assessed in the gastroenterology department of Pak-Emirates military hospital, Rawalpindi. Detailed history and examination was done. Relevant laboratory tests and an ultrasound abdomen were also carried out. Those with pancreatic lesions on ultrasound abdomen underwent EUS (endoscopic ultrasound). Amongst those undergoing EUS, 88 patients were found to have cystic pancreatic lesions. These 88 patients underwent detailed assessment with EUS-FNA (endoscopic ultrasound – fine needle aspiration) so that these pancreatic cysts could be characterized. Only some of the patients undergoing EUS-FNA had one or more of the worrisome features (solid component within the cyst, main pancreatic duct & gt; 5 mm in size, symptoms related to the cyst, family history of pancreatic cancer), and later underwent surgical resection. EUS was done with the patient in the left lateral decubitus position under intravenous sedation with midazolam. During the procedure, the patient was monitored using the cardiac monitor. Images of the pancreas, gallbladder and bile tree were obtained with the echoendoscope in the stomach and duodenum. Informed consent for the study and the endoscopic procedure was obtained from all patients. The study protocol was approved by the hospital ethics committee. Results: The study population included 50 females and 38 males. Many of these patients had one or more episodes of pancreatitis in the recent past. Most cystic lesions were found in the pancreatic body. The largest number of lesions were due to pancreatic pseudocysts. EUS was performed successfully in all patients. Findings have been summarised in the table according to gender. Conclusion: Identifying pancreatic cystic neoplasms is important since some have malignant potential. In that regard, EUS-FNA is a useful diagnostic modality and it can influence the management plan.References
Tanaka M, Fernández-del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology 2017;17(5):738–53.
Ardeshna DR, Cao T, Rodgers B, Onongaya C, Jones D, Chen W, et al. Recent advances in the diagnostic evaluation of pancreatic cystic lesions. World J Gastroenterol 2022;28(6):624–34.
Buerlein RCD, Shami VM. Management of pancreatic cysts and guidelines: what the gastroenterologist needs to know. Ther Adv Gastrointest Endosc 2021;14:26317745211045769.
Kim HS, Jang JY. Management Algorithms for Pancreatic Cystic Neoplasms. Arch Pathol Lab Med 2022;146(3):322–9.
Turner RC, Melnychuk JT, Chen W, Jones D, Krishna SG. Molecular Analysis of Pancreatic Cyst Fluid for the Management of Intraductal Papillary Mucinous Neoplasms. Diagnostics 2022;12(11):2573.
Chen W, Ahmed N, Krishna SG. Pancreatic Cystic Lesions: A Focused Review on Cyst Clinicopathological Features and Advanced Diagnostics. Diagnostics 2022;13(1):65.
Esposito I, Haeberle L. Nonmucinous Cystic Lesions of the Pancreas. Arch Pathol Lab Med 2022;146(3):312–21.
Chauhan SS, Abu Dayyeh BK, Bhat YM, Gottlieb KT, Hwang JH, Komanduri S, et al. Confocal laser endomicroscopy. Gastrointest Endosc 2014;80(6):928–38.
Lévy P, Rebours V. The Role of Endoscopic Ultrasound in the Diagnosis of Cystic Lesions of the Pancreas. Visc Med 2018;34(3):191–5.
Gaujoux S, Brennan MF, Gonen M, D’Angelica MI, DeMatteo R, Fong Y, et al. Cystic Lesions of the Pancreas: Changes in the Presentation and Management of 1,424 Patients at a Single Institution over a 15-Year Time Period. J Am Coll Surg 2011;212(4):590–600.
Valsangkar NP, Morales-Oyarvide V, Thayer SP, Ferrone CR, Wargo JA, Warshaw AL, et al. 851 resected cystic tumours of the pancreas: A 33-year experience at the Massachusetts General Hospital. Surgery 2012;152(3):S4–12.
Walsh RM, Vogt DP, Henderson JM, Hirose K, Mason T, Bencsath K, et al. Management of suspected pancreatic cystic neoplasms based on cyst size. Surgery 2008;144(4):677–85.
Spinelli KS, Fromwiller TE, Daniel RA, Kiely JM, Nakeeb A, Komorowski RA, et al. Cystic Pancreatic Neoplasms. Ann Surg 2004;239(5):651–9.
Misra D, Sood T. Pancreatic Pseudocyst. 2023. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024.
Seewald S, Ang TL, Teng KCYK, Soehendra N. EUS‐guided drainage of pancreatic pseudocysts, abscesses and infected necrosis. Dig Endosc 2009;21(Suppl 1):61–5.
Additional Files
Published
Issue
Section
License
Copyright (c) 2024 Faryal Riaz Khan Khan, Rao Saad Ali Khan, Ehtesham Haider, Fuad Ahmad Siddiqi, Muhammad Mehdi Hassan Naqvi, Salahuddin, Zara Riaz Khan

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Journal of Ayub Medical College, Abbottabad is an OPEN ACCESS JOURNAL which means that all content is FREELY available without charge to all users whether registered with the journal or not. The work published by J Ayub Med Coll Abbottabad is licensed and distributed under the creative commons License CC BY ND Attribution-NoDerivs. Material printed in this journal is OPEN to access, and are FREE for use in academic and research work with proper citation. J Ayub Med Coll Abbottabad accepts only original material for publication with the understanding that except for abstracts, no part of the data has been published or will be submitted for publication elsewhere before appearing in J Ayub Med Coll Abbottabad. The Editorial Board of J Ayub Med Coll Abbottabad makes every effort to ensure the accuracy and authenticity of material printed in J Ayub Med Coll Abbottabad. However, conclusions and statements expressed are views of the authors and do not reflect the opinion/policy of J Ayub Med Coll Abbottabad or the Editorial Board.
USERS are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles, or use them for any other lawful purpose, without asking prior permission from the publisher or the author. This is in accordance with the BOAI definition of open access.
AUTHORS retain the rights of free downloading/unlimited e-print of full text and sharing/disseminating the article without any restriction, by any means including twitter, scholarly collaboration networks such as ResearchGate, Academia.eu, and social media sites such as Twitter, LinkedIn, Google Scholar and any other professional or academic networking site.